During pregnancy, it’s easy to get so caught up in taking care of the baby and preparing for its arrival that you forget to take care of yourself. While your baby should certainly be a priority, it’s important to remember that keeping yourself healthy is just as much of a necessity—not just physically but mentally, too.
You’ve probably been warned about postpartum depression, but what about depression during pregnancy? Studies have shown that women are just as likely to suffer from depression during pregnancy as they are after. Furthermore, depression during pregnancy puts you at a higher risk for experiencing depression following the birth of your baby.
Keep reading for more information regarding depression and pregnancy, including:
- What causes depression during pregnancy
- Signs that you might be suffering from depression
- Finding the right treatment for you and your baby
What Causes Depression During Pregnancy?
Depression during pregnancy—also known as antepartum depression—is a mood disorder like any other form of depression. The American Congress of Obstetricians and Gynecologists estimates that as many as 23 percent of women experience symptoms of depression during their pregnancies.
During pregnancy, you become more sensitive to emotions, both your own and those of the people around you. This is a brain change that’s part of the way that your body prepares you for pregnancy and is meant to help you respond to your baby’s needs. However, these hormonal changes can also affect the chemistry of your brain and potentially result in depression.

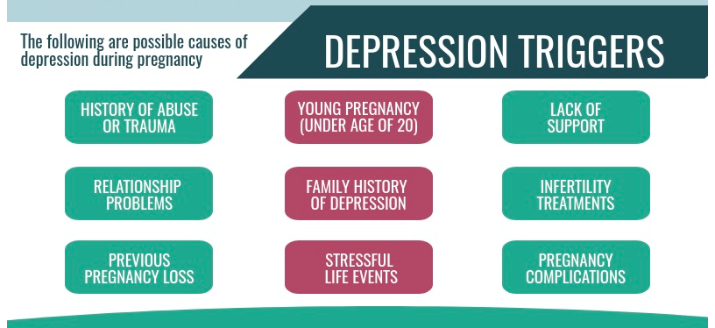
The medical community still isn’t totally sure what causes depression, but certain factors can increase your risk of experiencing depression during your pregnancy, including:
- You have had depression in the past.
- Your family has a history of depression or other mental health conditions.
- You have suffered from abuse or are currently living in an abusive environment.
- Your pregnancy was not planned or is not wanted.
- Other stressful events are currently taking place in your life right now.
- You have diabetes (pre-existing or gestational).
- You are experiencing complications with your pregnancy or have experienced complications with past pregnancies.
- You smoke, drink alcohol, or use harmful drugs.
Is There a Way to Prevent Depression During Pregnancy?
Unfortunately, there aren’t any guaranteed ways to prevent depression during pregnancy. However, counseling is considered to be effective in helping pregnant women who have an increased risk of depression. The U.S. Preventive Task Force recommends that you seek counseling if you are pregnant and identify with one or more of the following risk factors:
- Are having current feelings or symptoms of depression.
- Have a history of depression or other mental health conditions.
- Are a teenager or single mother.
- Are experiencing other stressful life events.
- Are a victim of intimate partner violence.
Warning Signs of Depression During Pregnancy
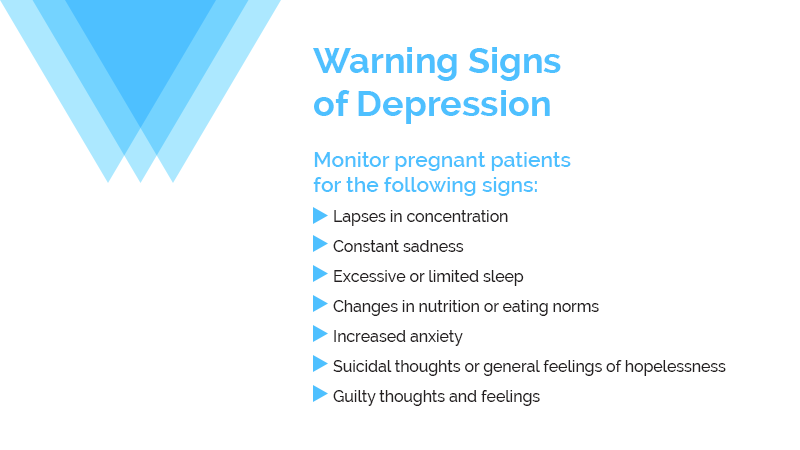
The warning signs and symptoms of depression during pregnancy are the same as those that are used to identify depression in other instances as well. These include:
- Feeling persistently sad, hopeless, overwhelmed, restless, or moody.
- Excessive crying.
- Feelings of guilt or worthlessness.
- Thinking of death, suicide, or hurting yourself or your baby.
- Feeling like you’re in a fog or out of touch with your surroundings.
- Difficulty remembering things, concentrating, or making decisions.
- Not being able to sleep (insomnia) or sleeping too much (hypersomnia).
- Withdrawing from family and friends.
- Not having an interest in activities that you used to enjoy.
- Having no energy or feeling tired all of the time, regardless of how much sleep you get.
- Having inexplicable headaches, stomach aches, or any other kind of physical pain.
What’s Not Normal?
While diagnosing depression in pregnant women is not a different procedure than diagnosing depression in someone who is not pregnant, depression in pregnant women is often overlooked because there are so many similarities between depression and the emotional side effects of pregnancy. This makes depression during pregnancy especially dangerous.
Because you’ll be experiencing so many hormonal changes that can result in mood swings, increased irritability, and random crying, it can be difficult to figure out which feelings are “normal” to have during pregnancy and which ones are not. If you have a history of depression, you might be able to identify some similarities between your current feelings and past episodes. However, if you have never experienced depression before, you might have no idea what to look for.
Symptoms of depression last for at least two weeks. You might find it beneficial to keep a mood journal during your pregnancy (and afterward) to track your mood in order to differentiate between bad days and persisting warning signs.

It’s important to remember that suicidal thoughts, while nothing to be ashamed of, are never “normal” and should not be dismissed as invalid or something that you should be forced to deal with. Feeling suicidal—whether actively thinking of committing suicide or having more passive thoughts that life is not worth living—is a serious indication of depression, and you should seek medical attention immediately if you are thinking of harming yourself or your baby.
Depression Treatment Options When You’re Pregnant
Treating depression is always a complex process for a multitude of reasons. Firstly, depression is a complicated disorder that affects each individual differently. Additionally, there are a variety of routes that can be taken in terms of treatment methods, and there’s no way to know which method will be most effective before trying it. This means that treating depression can be a long, arduous journey that involves a great deal of trial and error.
When it comes to treating depression during pregnancy, there are, of course, more factors that need to be considered than there would be with a non-pregnant patient. Ultimately, it’s up to the patient to decide how they want to proceed with their treatment.
Psychotherapy
As previously discussed, counseling—formally known as psychotherapy—is considered an effective means of treating depression during pregnancy. There are various types of therapy, and most therapists utilize a mix of approaches depending on the patient.
Cognitive-Behavioral Therapy
Cognitive-behavioral therapy examines a patient’s thought process in order to find and replace unhealthy thinking patterns. Goal-oriented with a focus on problem-solving, this approach involves changing behavior and emotional reaction through practice and discussion.
Psychodynamic Therapy
Psychodynamic therapy aims to understand how past events in a patient’s life might be influencing them in the present. By increasing self-awareness, this approach can help a patient develop healthier habits by having a better understanding of themselves.
Conjoint Therapy
Conjoint therapy is a form of therapy in which two (or more) patients are seen at once in order to build communication skills and strengthen a relationship. This type of treatment can be beneficial for expecting parents who are struggling to communicate with each other or who simply want to better their relationship before the birth of their child.
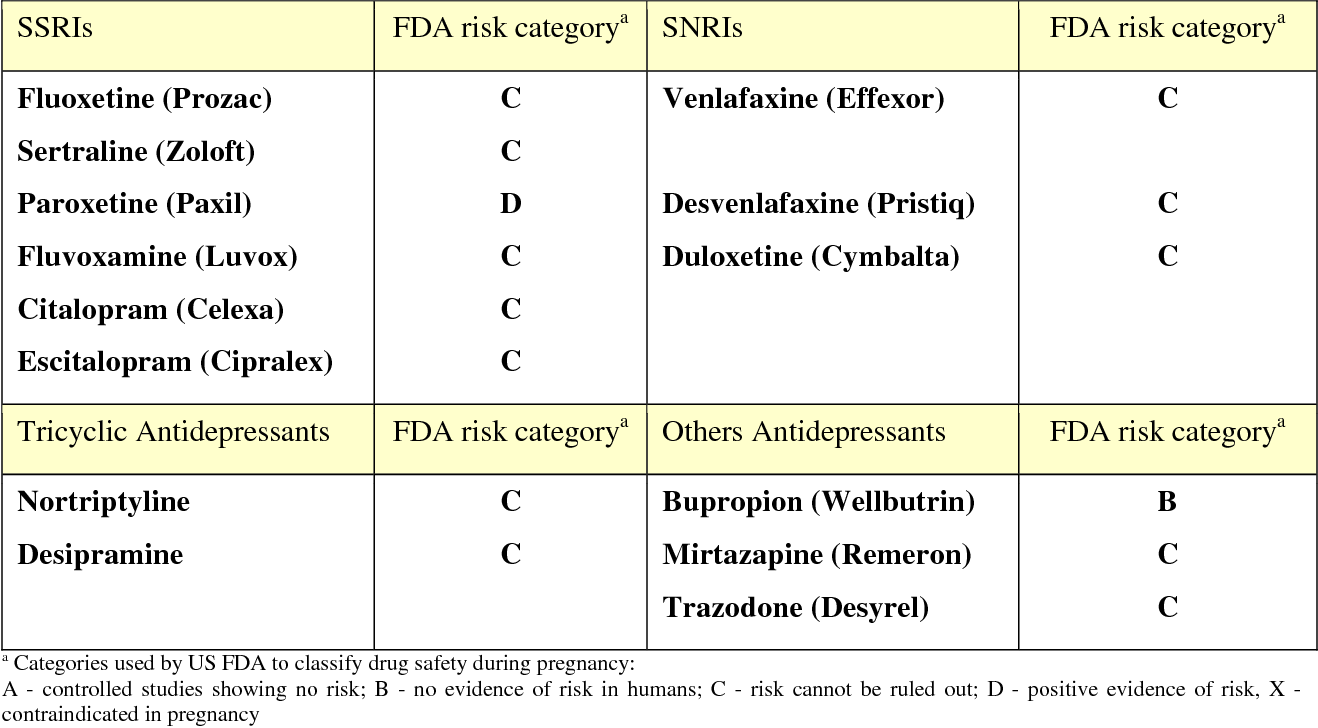
Pharmaceutical Treatment
Some antidepressants are considered safe to take while pregnant, and if you are already taking an antidepressant when you become pregnant, depending on the medication, your doctor might recommend that you continue to take it throughout your pregnancy. There are some risks associated with taking antidepressants during pregnancy, especially during the third trimester.
Non-Pharmaceutical Treatment
Though therapy and antidepressants are usually the first line of treatment for any kind of depression, these methods aren’t always effective. Additionally, if you start to experience depression while pregnant, you might be reluctant to start taking antidepressants. Fortunately, there are non-pharmaceutical options that are available in these circumstances.
Electroconvulsive Therapy
Electroconvulsive therapy (ECT) uses electrical currents to stimulate the brain and help relieve symptoms of depression. Though non-pharmaceutical, ECT is a full medical procedure during which the patient is unconscious and must be driven to and from the hospital for the operation and supervised afterward.
ECT should not have any effect on your baby—however, extra precautionary measures will need to be taken to undergo ECT while pregnant, such as the use of a fetal heart monitor, and your doctor might opt for intubation rather than anesthesia after the first trimester.
Transcranial Magnetic Stimulation
Transcranial magnetic stimulation (TMS) is like ECT in that it is a form of brain stimulation—however, it uses magnetic pulses rather than electric shocks. Unlike ECT, TMS is non-invasive, and the patient is fully conscious throughout the treatment. TMS also has fewer risks than ECT and is generally considered to be a safe, less extreme form of treatment.

TMS requires consistent application on a daily basis (typically five days a week) for around six weeks. While the length of each session varies from patient to patient, the average duration is approximately 30 minutes.
Like ECT, TMS is safe for pregnant women, and it should not impact the baby or nursing. Because TMS is overall more tolerable and does not involve sedation or a surgical procedure, pregnant patients might prefer to try TMS before attempting ECT.
Treating Your Depression Is Critical to Your Baby’s Health
It’s important to remember than depression during pregnancy doesn’t just affect you—it can also affect your baby, especially if you do not seek treatment. Potential dangers of untreated antepartum depression include premature delivery, low birth weight, and even miscarriage. It also puts you at a higher risk for developing postpartum depression, which can mean trouble bonding with your baby and in extreme cases, lead to them living in an unsafe environment.
The hopelessness that comes with depression might make you feel as though getting better is not a possibility. However, this notion, no matter how profound, is fully inaccurate. The first step toward recovery is telling someone, whether it’s your partner, friend, family member, or a medical professional. You are not obligated to suffer in silence, nor should you. Find help—for you and your baby.










