When mentioning electric shock therapy, now know as Electroconvulsive Therapy (ECT), many people will picture gruesome scenes from cultural depictions, like Jack Nicholson’s character in One Flew Over the Cuckoo’s Nest, where he receives the therapy as punishment instead of treatment. There are many other cultural references of a similar nature, more recently the Beth Dawes character on Mad Men, who seemed to have lost all memory of her recent affair with Pete Campbell. Critics have gone so far as labeling ECT as abuse, while psychiatrists, and their patients, find it safe and effective. There are few medical treatments that share such disparaging perceptions.

Today’s use of ECT and other brain stimulations are a far cry from these depictions. For instance, patients receiving ECT are now sedated to avoid any experience of potential pain during treatment.

For the 30 percent of the population suffering from depression that don’t respond to pharmacological treatment, brain stimulations are life changing. The treatments involve applying electric or magnetic energy on specific regions of the brain to adjust the function of neural circuits. This helps relieve symptoms of depression or other treatment resistant mental illnesses like bipolar disorder.
History of Brain Stimulations
Invented in the late 1930s in Italy, ECT induced seizures in patients to ease symptoms of mental illness. While this may seem counterintuitive, there are many medical treatments that require painful experiences for therapeutic purposes, like chemotherapy to fight cancer. Before ECT doctors used chemicals to induce the seizures, specifically Metrozal, but patients were so resistant to the drug they often had to be chased to administer it, claiming it evoked feelings of terror right before the seizures. And while culturally ECT was depicted as terrifying itself, it was actually invented as a safer, less fearful way of inducing the seizures. At the time doctors felt this was achieved and within a few year of its invention is was widely used around the world for treatment.

The use of ECT in the 1950s certainly contributed to it’s stigma. Many hospitals used treatment as a threat to maintain control of their wards, and at that time there was no anesthesia or muscle relaxers used to ease the discomfort of treatment. At that time ECT was also used to “treat” homosexuality, which we now know is not an illness at all, therefore the treatment provide no benefit to the “patients.” Fortunately this practice did not last since there was no evidence it could alter an individual’s sexuality. That doesn’t change the impact such use had in stigmatizing the treatments.
Modern Brain Stimulations
Today there are four additional types of brain stimulation beyond ECT including, Repetitive Transcranial Magnetic Stimulation (rTMS), deep brain stimulation (BDS), vagus nerve stimulation (VNS), and magnetic seizure therapy (MST).
Repetitive Transcranial Magnetic Stimulation
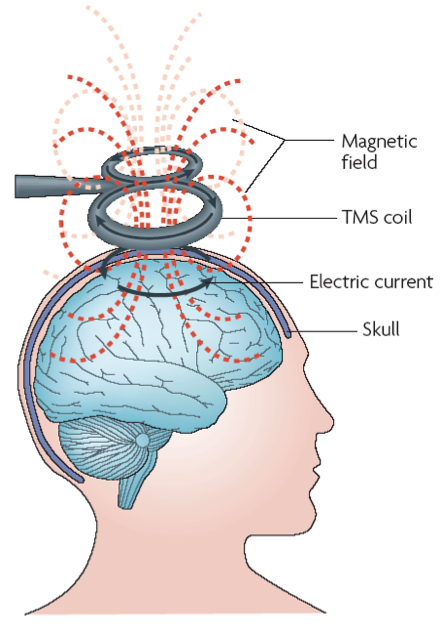
Introduced in 2008, rTMS is the least invasion option and has been approved by the FDA for treatment of depression, and more recently obsessive compulsive disorder. Using an electromagnetic coil, it delivers short electromagnetic pulses to specific areas of the brain. During treatment patients are awake and typically feel no pain and no cognitive side effects. Potential side effects are minimal including tingling in the jaw, face or scalp; headaches, and slight discomfort at application site. There is a rare side effect of possible seizures so individuals at risk of seizures are advised to avoid this treatment.
While still a young treatment initial research is promising with 30% of recipients experiencing less depressive symptoms. There is a great deal of research currently for other possible treatments including eating disorders, PTSD, and addiction.
Vagus Nerve Stimulation
Originally developed to treat epilepsy, Vagus Nerve Stimulation (VNS) involves implanting a pulse generator in the upper chest, which connects to the vagus nerve. The vagus nerve runs from the abdomen to the brain. VNS was approved to treat depression in 2005 by the FDA. Patients typically note an improvement with treatment when combined with antidepressants, but it’s noted the typically don’t completely disappear, like with treatments such as TMS. It also may take several months to notice any effect, and side effects include discomfort at implant site, voice changes, sore throat, breathing issues and trouble swallowing. It should also be noted, due to the invasiveness this is typically a last resort treatment after at least 4 other treatments have failed, and in some cases it can actually worsen symptoms.

Deep Brain Stimulation
While not approved for treating depression yet, Deep Brain Stimulations (DBS) it is approved for OCD, and was mainly used to treat Parkinson’s disease. Like VNS, it utilizes pulse generators, but rather than short bursts, it’s a continuous stimulation. Implants are placed on both sides of the brain and chest. Patients are actually awake, but numbed during the brain procedure. It’s believed DBS helps reset the area of your brain having issues. Possible side effects include infection, confusion, mood changes, movement issues, lightheadedness, trouble sleeping, and in more severe cases, brain bleeding or stroke. While it’s not yet approved, is does show promise in depression treatment, but once again due to its invasiveness, it would likely only be used once other treatments have failed.

Magnetic Seizure Therapy
The newest brain stimulation treatment, Magnetic Seizure Therapy (MST), is a cross between ECT and TMS. Like ECT it stimulates seizures, but like TMS it does so using magnetic pulses over the areas of the brain related to mental illness. Since the pulses are more intense than TMS, patients need anesthesia and muscle relaxer like with ECT. The only known side effects are those related to the anesthesia and seizures, but it’s still very early. More research is needed to determine how best to administer treatment, but early research has shown 40 to 60 percent of those with treatment resistant depression and bipolar disorder responded to MST, with 15 to 30 percent experiencing significant relief.

While brain stimulations are not a first round treatment for those dealing with mental health issues they show great progress in address the large percentage of individuals who do not respond to first line treatment, and scientists are just scratching the surface of what’s possible in treating a range of ailments with brain stimulation. They’ve come a long way from their previous reputation and will likely continue to improve and evolve.










